HELLO GUYS, This is an online e log book to discuss our patient de-identified health data shared after taking his/her/guardians signed informed consent.
Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evidence based input
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
ADMITTED ON 29/10/21(FRIDAY)
A 22 YRS OLD FEMALE CAME TO THE CASUALITY WITH
C/O RASHES OVER BODY WITH ITCHING SENSATION SINCE 4 DAYS
FEVER SINCE 8 DAYS BACK, HIGH GRADE A/W CHILLS DECREASED ON MEDICATION
A/W GENERALISED BODY PAINS+
H/O HERBAL MEDICATION ON THE (TUESDAY)
F/B RASHES OVER THE LIMBS /BODY NEXT DAY
NO H/O COLD, COUGH
H/O GENERALISED EDEMA ALL OVER THE BODY SINCE 3DAYS
NO H/O DECREASED URINE OUTPUT AND ABDOMINAL DISTENSION
PATIENT SAYS THAT SHE HAVE TAKEN HERBAL MEDICATIONS FOR JAUNDICE
(WENT TO HERBAL PRACTITIONER WITH C/O FEVER ON AND OFF FOR 10 DAYS AND 2 DAYS VOMITING EPISODE)
PAST HISTORY:
N/K/C/O DM,TB,ASTHMA,CVA,
CAD, EPILEPSY
PERSONAL HISTORY:
APPETITE: NORMAL
DIET: VEGETARIAN
NO ANY ADDICTION
REGULAR BOWEL AND BLADDER MOVEMENTS
ADEQUATE SLEEP
GENERAL EXAMINATION:
PT IS C,C,C
PALLOR - PRESENT
GENERALISED EDEMA -PRESENT
RASHES PRESENT ALL OVER THE BODY
NO ICTERUS, CYANOSIS, CLUBBING, LYMPHADENOPATHY,
VITALS:
TEMP- 101 F
PULSE- 120 bpm
RR- 20 cpm
BP- 90/70 mmHg
SPO2- 99@ROOM AIR
GRBS- 86 mg/dl
SYSTEMIC EXAMINATION:
CVS: S1S2 ,NO MURMURS
RS: BAE+,NVBS+
CNS: NFD
P/A: SOFT, NON-TENDER
INVESTIGATIONS:(29/10/2021)
1)HEMOGRAM:
2)CUE:
3)BLOOD GROUP:
4)PT,INR:
5)APTT:
6)LFT:
7)RFT:
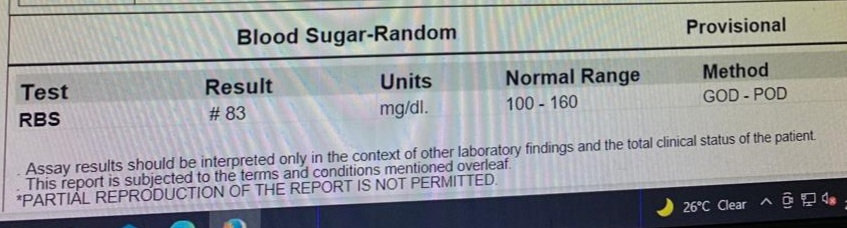
8)RBS:
9)RAPID DENGUE TEST:
10)ECG:
11)USG ABDOMEN:
-GALLBLADDER EDEMA,
-MILD SPLENOMEGALY
-MINIMAL ASCITES
DVL REFERRAL DONE:
OUTSIDE REPORTS:
DIAGNOSIS: DRUG INDUCED RASH
TREATMENT:
1.T.UDILIV 300mg PO/BD
2.SYRUP. LACTULOSE 15ml PO/OD IN NIGHT
3.T.ATARAX 25mg PO/OD IN NIGHT
4.T.PCM 500mg PO/SOS
INVESTIGATIONS ON DAY2(30/10/2021):
HEMOGRAM
RETICULOCYTE COUNT:
LFT:
LDH:
CRP -POSITIVE
DAY-3:
Soap notes
Icu 6th bed:
S:
1 Fever spike at 4:00am
Itching decreased
Rashes present
O:
PR: 82bpm
Bp: 120/80mmhg
Temp: 99F
RR:18cpm
Cvs:s1,s2heard
Rs:BAE+
CNS:NFD
Generalised edema present.
Rashes present all over the body
A:
Hepatitis secondary to Drug induced(herbal medication)
P:
1)Tab.UDILIV 300mg PO/BD
2)SYP.Lactulose 1ml/po/H/s
3)Tab.ATARAX 25mg PO/OD/Hs
4)Tab.RIBOFLAVIN 10MG PO/BD
5)Tab.PCM 500mg PO/SOS
6)Tab.Zincovit po/od
DAY-4 (1/11/021)
Soap notes
Icu 6th bed:
S:
Fever spikes present the while night
Itching has decreased
Rashes present
O:
PR: 82bpm
Bp: 120/80mmhg
Temp: 98.1F at 7am
RR:18cpm
Cvs: S1,S2 heard
Rs: BAE+
CNS:NFD
Generalised edema present.
Rashes present all over the body
A:
Hepatitis secondary to Drug induced(herbal medication)
P:
1)SYP.Lactulose 15ml/po/H/s
2)Tab.ATARAX 25mg PO/OD/Hs
3)Tab.RIBOFLAVIN 10MG PO/BD
4) Tab.PCM 500mg PO/SOS
5) Tab.Zincovit po/od