Medicine case discussion
Saturday, 28 May 2022
Ascitic tap
Pleural tap
"This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment
Pleural tap:
Performed pleural tap for a patient with pleural effusion on 09/10/2021 under the guidance of Dr. Vinay
Performed pleural tap for a patient with pleural effusion on 29/01/22 under the guidance of Dr. Sai charan
Coffee coloured vomitus
"This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment
Ryles aspiration: coffee coloured vomitus
Performed ryles aspiration for a patient with coffee coloured vomitus on 09/10/2021 under the guidance of Dr. Pradeep
Friday, 21 January 2022
55 yrs old female with CKD with secondary to frature
"This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment"
A 55 year old female , agricultural labourer by occupation ,resident of nalgonda, came to the opd with chief complaints of
1)facial puffiness since 15 days
2)pedal edema since 15 days
3) shortness of breath since 15 days
HOPI
The patient was apparently asymptomatic 7 years back then she was diagnosed with hypertension.and on irregular medication
5 years back she had trauma to her left hand (fracture)for which she took treatment in govt hospital, In her routine investigations her cretinine levels were found to be high and they were referred to Kims.She was prescribed medications for the same.
3 years back, she went to local rmp for her knee joint pains, for which she was prescribed pain medication which she used them for one year.
15 days back she gradually developed facial puffiness, bilateral pedal edema (pitting type)up to knee joint and shortness of breath ,grade 3.
She also complains of deceased urine output during the day,nocturia, constipation.
Past history:
K/C/O HTN since 7 years
On irregular medication
Personal history:
Diet -mixed
Appetite-decreased
Sleep-adequate
GENERAL PHYSICAL EXAMINATION:
Patient is conscious, coherent, cooperative, moderately built and nourished.
No pallor,icterus ,cyanosis,clubbing, lymphadenopathy
Bilateral pedal edema (pitting type)+
VITALS:
Bp-180/90mmhg
Pr-92bpm
Rr-20cpm
Spo2 -98% at RA
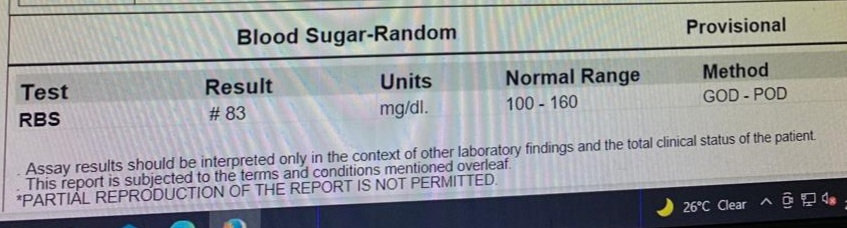
Grbs-101mg/dl
Systemic examination:
Cvs-S1,S2 +
Rs-Bae+,nvbs+
P/A- soft ,nontender
Cns- nad
Diagnosis :
Chronic kidney disease ? Secondary to frature heart failure(Renocardiac syndrome)

Treatment:
One round hemodialysis was done on 20/01/2022
1) neb with duolin 4 respules/ stat
2) INJ. LASIX 40 MG IV /BD
3) TAB. NODOSIS 550 MG PO/BD
4) TAB.SHELCAL PO/OD
5) TAB.OROFER XT PO/BD
6)INJ.ERYTHROPOIETIN 4000 IU S/C WEEKLY ONCE
7)TAB. NICARDIA 20 mg PO /BD
8)INJ HAI 12U IN 25% DEXTROSE/IV/OVER 30MINS
Day2: soap notes
S:sob resolved after hemodialysis
Pedal edema slightly reduced
Constipation -
O: bp :150/90 mmhg
Pr: 85 bpm
Rr: 20 cpm
Spo2:
A: Chronic kidney disease ? Secondary to frature heart failure(Renocardiac syndrome)
P:
INJ. LASIX 40 MG IV /BD
TAB. NODOSIS 550 MG PO/BD
TAB.SHELCAL PO/OD
TAB.OROFER XT PO/BD
INJ.ERYTHROPOIETIN 4000 IU S/C WEEKLY ONCE
TAB. NICARDIA 20 mg PO /BD
INJ HAI 12U IN 25% DEXTROSE/IV/OVER 30MINS
DAY 3 soap notes
S: complaints of sob from early morning
Dry cough since yesterday night
O:
bp :170/100
Pr: 94 bpm
Rr: 24 cpm
Spo2: 96% at RA
A: Chronic kidney disease with hyperkalemia
P: neb duolin stat given
planning for dialysis as she is complaining of sob
1) neb with duolin 4 respules/ stat
2) INJ. LASIX 40 MG IV /BD
3) TAB. NODOSIS 550 MG PO/BD
4) TAB.SHELCAL PO/OD
5) TAB.OROFER XT PO/BD
6)INJ.ERYTHROPOIETIN 4000 IU S/C WEEKLY ONCE
7)TAB. NICARDIA 20 mg PO /BD
8)INJ HAI 12U IN 25% DEXTROSE/IV/OVER 30MINS
9) SYP . Ascoryl D 10 ml po / TID
Soap notes day 4:
S:Sob resolved after hemodialysis
Facial puffiness-
Pedal edema reduced
Cough resolved
O:
bp:160/90 mmhg
Pr: 84bpm
Rr: 20cpm
Sp02: 98%at RA
A: Chronic kidney disease ? Secondary to frature heart failure(Renocardiac syndrome)
INJ. LASIX 40 MG IV /BD
TAB. NODOSIS 550 MG PO/BD
TAB.OROFER XT PO/BD
INJ.ERYTHROPOIETIN 4000 IU S/C WEEKLY ONCE
TAB. NICARDIA 20 mg PO /BD
INJ HAI 12U IN 25% DEXTROSE/IV/OVER 30MINS
Tab. ATENAM sos OD
Sunday, 14 November 2021
60 yrs old with Heart failure with preserved ejection fraction (ef:42%) with chronic kidney disease with type 2 DM and HTN
HELLO GUYS, This is an online e log book to discuss our patient de-identified health data shared after taking his/her/guardians signed informed consent.
Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evidence based input
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
UNIT 5 admission:
A 60 year old man presented at 9:10PM to casualty with c/o
- SOB since 4pm today
-cough since 4pm
Patient presented with c/0 sudden onset of dyspnea since 4pm today with productive cough since 4pm today.He was apparently asymptomatic 25years back after which he got diagnosed to be a diabetic . He was on irregular medications also gives h/0 LOC while going to washroom . Regular alcoholic since 10years -consumes 90-180ml whiskey/day.last alcoholic consumption was 5years back . Gutka consumption 10years back for 20years
5years back - B/L pedal Edema-diagnosed with CKD
2years back -SOB on supine position , relieved on sitting posture along with B/L pedal Edema.
1year back - SOB (grade 4). H/O CAD in January ?MI
February- presented to our casualty with SOB and was diagnosed with HFPEF and also k/c/o ckd(diagnosed 5years back when patient developed B/L pedal edema).
On 18/10/21- he came with SOB since 2 hours along with right sided chest pain since 2hrs.
Vitals at admission :
Temperature: a febrile
PR-86 bpm
RR-26cpm
BP-150/90 mmhg
Sp02- 92% at RA
GRBS- 151 mg%
General examination :
Pallor - PRESENT
Icterus,cyanosis,lymphadenopathy,clubbing,oedema of feet,dehydration- ABSENT
Systemic examination. :
CVS -
JVP - present
Apex beat -6th ics at mcl
S1s2 - heard
RS-
Inspiratory crepts in B/L IMA, IAA, ISA
DIAGNOSIS:
-HFPEF with CKD
-k/c/o type 2 DM since 25 years
-k/c/o HTN since 10 years
DAY 1:
SOAP NOTES :
ICU 2nd BED.
S: fever spike , SOB reduced.
O: pt is conscious , coherent , cooperative BP:100/80mmhg. Temp : 101F, PR:116 bpm , spo2:98%on 4L02. CVS: S1S2 heard , RS:BAE+,B/L crepts IAA, ISA , P/A: soft , non tender , CNS: HMF intact , NAD.
A : HFREF(EF:42%) with MODERATE LV dysfunctional, CKD(stage V), DM+ , HTN+. P:
1.Head end elevation up to 30degree 2.02 supplementation
3.fluid restriction less than 1 litre per day
4. salt restriction
5.inj. LASIX 40mg/IV/BD
6.tab.CARDIVAS 3.125 mg PO/OD
7.tab. VILDAGLIPTIN 50mg PO OD 8.tab.TAMSULOSIN-D 0.4mg PO OD
9.tab. NODOSIS 500mg PO BD 10.tab.ECOSPRIN-AV 75/20 mg OD
11.tab. HYDRALAZINE 12.5mg PO OD
12.Neb with IPRAVENT , BUDECORT
13.Syp. ASCORYL 10ml PO TID
14.DAILY WEIGHT MONITORING
15.STRICT I/O CHARTING
16.MONITOR VITALS
DAY 2:
SOAP NOTES : AMC CUBICLE BED.
S: no fresh complaints, NO fever spikes.
O: pt is conscious , coherent , cooperative
BP:100/80mmhg.
Temp : 101F,
PR:116 bpm ,
spo2:98%on RA.
CVS: S1S2 heard ,
RS:BAE+,B/L crepts IAA, ISA ,
P/A: soft , non tender ,
CNS: HMF intact , NAD.
A : HFREF(EF:42%) with MODERATE LV dysfunctional, CKD(stage V), DM+ , HTN+.
P:
1.Head end elevation up to 30degree 2.02 supplementation if spo2 <95
3.fluid restriction less than 1 litre per day
4.salt restriction
5.inj. LASIX 40mg/IV/BD
6.tab.CARDIVAS 3.125 mg PO/OD 7.tab. VILDAGLIPTIN 50mg PO OD 8.tab.TAMSULOSIN-D 0.4mg PO OD
9.tab. NODOSIS 500mg PO BD 10.tab.ECOSPRIN-AV 75/20 mg OD
11.tab. HYDRALAZINE 12.5mg PO OD
12.Neb with IPRAVENT , BUDECORT
13.Syp. ASCORYL 10ml PO TID
14.DAILY WEIGHT MONITORING
15.STRICT I/O CHARTING
16.MONITOR VITALS
17.T.OSELTAMAVIR 75mg PO BD
PLANNING FOR DISCHARGE
He got admitted with us twice
First admission in February elog
https://jeeharikasahu.blogspot.com/2021/02/60-year-old-male-with-complaints-of.html?m=1
Second admission elog - in October
https://roshnajilla.blogspot.com/2021/09/60year-old-male-with-hfpef.html?m=1
This is his third admission
https://ranjith119.blogspot.com/2021/11/hello-guys-this-is-online-e-log-book-to.html
Sunday, 31 October 2021
22 YRS OLD FEMALE WITH DURG INDUCED RASH
HELLO GUYS, This is an online e log book to discuss our patient de-identified health data shared after taking his/her/guardians signed informed consent.
Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evidence based input
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.